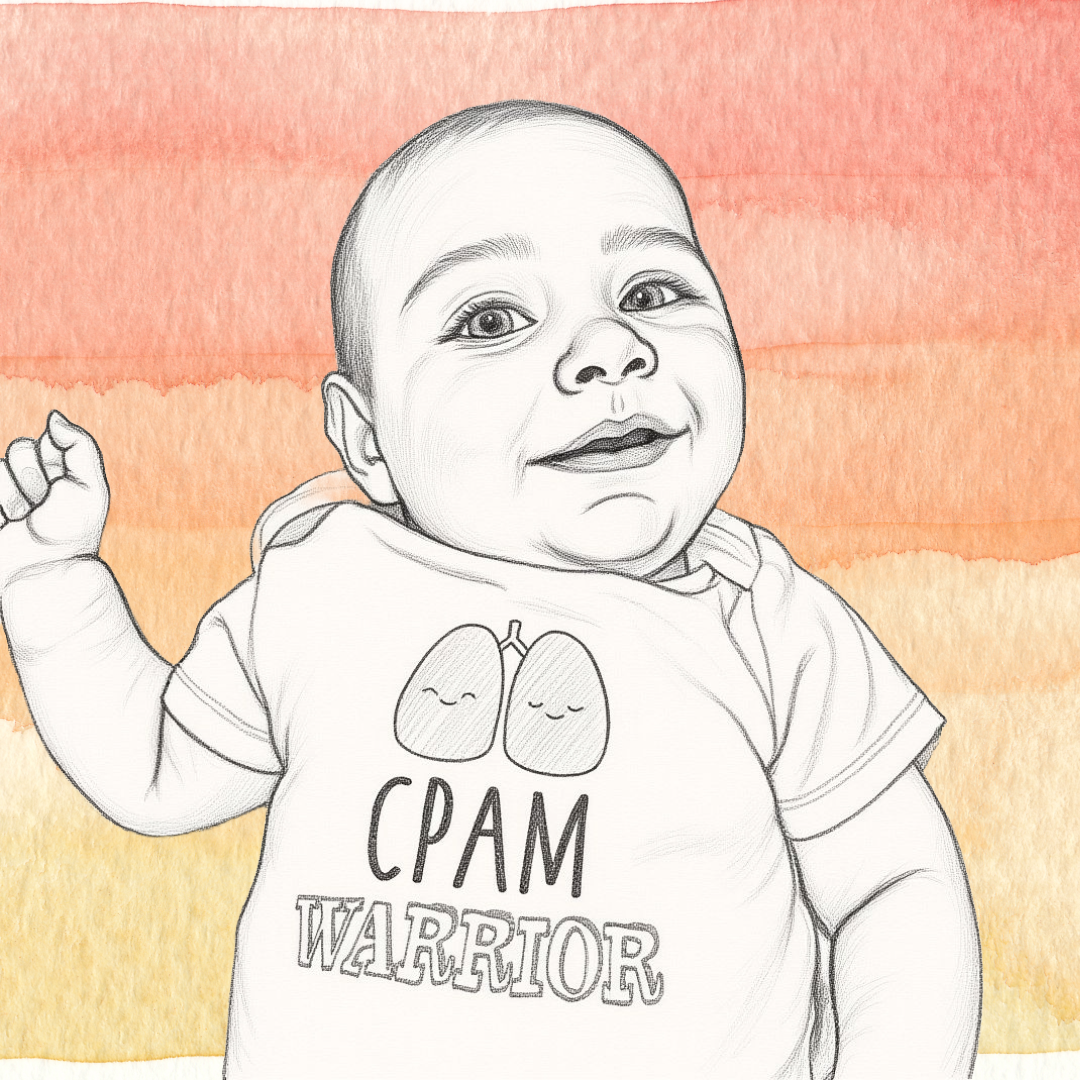
7/ Evan’s Story
Terrified after a prior scan scare, Evan’s parents heard “we need the doctor” and learned their baby had a lung malformation with a large feeder vessel. Although prenatal imaging later looked clear, a CT at two months revealed major blood diversion. Surgery at 2.5 months was hard, but he recovered and is thriving.
Our story really began with our previous pregnancy. We’d had an issue at our anatomy scan so I went into this scan terrified. All seemed to be going well, they weren’t spending extra time on any one area and I thought we were in the clear until I heard the dreaded words “we just have to get the doctor”. My heart stopped because I already knew that meant there was a problem.
When the head of MFM walked into my room I couldn’t breathe. He told us our baby had what looked like a CPAM. His heart was shifted and being compressed and it looked like there was a very large feeder vessel (note: a feeder vessel indicates a hybrid lesion or a pulmonary sequestration). He told us we would be having biweekly scans and sent us for a fetal echo. I immediately started googling, trying to understand what was going on and why this happened. As I came to find out, this wasn’t anything that I did or didn’t do. It is random.
We continued MFM appointments although as I got further along the mass was no longer visible. The fetal echo appeared clear and they couldn’t find this feeder vessel the MFM had kept seeing. We met with NICU and our surgeon. At this point, we were told it was a 50/50 chance he would need immediate intervention at birth. Surgery was optional but we were leaning towards it to prevent any future complications. My surgeon had a vacation scheduled so we scheduled an induction just in case my son needed him.
He was born at 38.5 weeks with an entire team at my bedside. That first cry was the most beautiful sound I ever heard. I sobbed. He was ok and breathing. It was a relief because that wasn’t something we were promised. He had another echo done and a chest X-ray, both of which appeared clear so we were sent home.
We met with our surgeon again and he ordered a CT scan. He had prepped us that X-rays are often clear so we needed the CT which was scheduled for around 2 months old. At this point we thought he was asymptomatic besides eating constantly, not pooping and never sleeping but I thought that was normal baby stuff. We went to the CT scan hungry, they put in the IV and I was able to nurse and swaddle him. He went right to sleep and that was actually super easy.
We had an appointment scheduled with our surgeon for later that day to review the results. At that point they saw the huge feeder vessel and he stated he was shocked that my son wasn’t in heart failure. The vessel was the size of an adult pinky and coming straight off his aorta. Half of his blood volume was being diverted directly to the mass. They sent us immediately for another echo and booked surgery. That echo again was ok. He wasn’t in heart failure but the energy he was using to pump blood was likely explaining the constant hunger and not sleeping. Surgery was no longer optional.
We brought him in at 2.5 months old. Handing him off to the surgeon was the hardest thing I have ever done. I was terrified. Those hours he was in surgery were agonizing. We sat in the PICU listening for any mention of our son. Finally 5 hours later we heard his name. He was brought up by an entire team, on oxygen and very sedated. They had done an open lower left lobectomy and were happy they had been able to extubate him in the OR. He had a chest tube and tons of monitors. Those first 24 hours were rough. He was in a lot of pain, IV morphine helped but he was so out of it and couldn’t eat.
We struggled being in the PICU around parents whose children were extremely sick. It was a hard experience: I felt awful and guilty being upset about my son even though I knew he was coming home in a few days, which was not the case for every parent there.
By the next morning, he was so much better. He was smiling and transitioned to Tylenol for pain management. He still was not eating much. My hospital had provided a breast pump as I was pumping. We were able to give him some bottles. It was hard to nurse with the chest tube and all the monitors. The hospital also provided meal trays for me as a breast-feeding mom, which was nice.
We were moved to the regular pediatric floor on day two. We stayed there for a few more days with the chest tube on suction. They then stopped the suction, but he had a lot of drainage still. The original plan was to stop suction for 24 hours and then remove it, but because he had so much drainage we waited an extra day. On that final day, they removed the chest tube, did one more chest X-ray, and we were free to go. By that point, he was totally himself again. We went home with just some Steri-Strips and really no restrictions. Just not to scrub the surgical site and allow the strips to fall off naturally.
Our surgeon and final pathology later confirmed the mass had characteristics of both CPAM and pulmonary sequestration, indicating a hybrid lesion. We had a few postop appointments, but were discharged from all specialists before he turned one. That first winter he got sick a lot. Every cold seemed to turn into pneumonia, but since then, he has been a normal healthy kid. This entire experience was beyond draining. I am a nurse and familiar with medical stuff. My husband looked to me for answers that I just didn’t have this time. Fellow CPAM parents were my saving grace. Their stories, advice and support got me through this. Today it is just a memory. Occasionally I catch a glimpse of his faded scars and have a wave of emotions. My son is a happy and healthy child. He plays sports, runs, swims and keeps up with his peers and siblings.
Evan today–happy, healthy, active!